Hereditary Tyrosinemia Type 1 (HT-1) is a rare genetic disorder characterized by the deficiency of the enzyme fumarylacetoacetate hydrolase (FAH), which is essential for the breakdown of the amino acid tyrosine. Without this enzyme, toxic byproducts build up in the body, leading to severe liver and kidney damage, as well as other complications if left untreated.
Medicine for this genetic disorder disease. Please fill out the form below to receive an instant quote.
Prevalence: HT-1 is considered a rare disease, with an estimated prevalence of approximately 1 in 100,000 to 1 in 120,000 live births worldwide. However, the prevalence may vary among different populations and regions.
Inheritance: HT-1 is inherited in an autosomal recessive manner, meaning both parents must carry a mutated gene for the condition to develop in their child. If both parents are carriers, there’s a 25% chance with each pregnancy that their child will have HT-1.
Hereditary Tyrosinemia Type 1 (HT-1) often occurs more frequently in countries like Lebanon, Quebec (Canada), and some regions of Scandinavia.
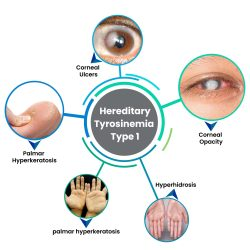
Symptoms of HT-1:
The symptoms of HT-1 can vary widely among individuals but may include:
- Liver problems: Jaundice (yellowing of the skin and eyes), enlarged liver, liver failure.
- Kidney problems: Kidney tubular dysfunction, kidney stones.
- Neurological symptoms: Poor growth, developmental delays, tremors, seizures.
- General symptoms: Poor appetite, vomiting, diarrhea, and a cabbage-like odor to the urine, sweat, and breath.
Causes of Hereditary Tyrosinemia (HT-1): Hereditary tyrosinemia type 1 (HT-1) is caused by:
- Genetic Mutation: Hereditary Tyrosinemia (HT-1) is caused by a genetic mutation. This means that a person inherits the condition from their parents through their genes.
- Faulty Enzyme: The genetic mutation affects the production of an enzyme called fumarylacetoacetate hydrolase (FAH). This enzyme is essential for breaking down a substance called tyrosine, which is found in many foods.
- Accumulation of Harmful Substances: When the FAH enzyme is not working properly due to the genetic mutation, tyrosine, and its byproducts start to build up in the body. This accumulation can damage the liver and other organs, leading to the symptoms of Hereditary Tyrosinemia.
Diagnosis:
HT-1 is usually diagnosed through newborn screening tests or when symptoms appear in infancy. Diagnostic tests may include blood tests to measure levels of tyrosine and its byproducts, urine tests to detect abnormalities, and genetic testing to confirm the presence of mutations in the FAH gene.
Treatment:
Early diagnosis and treatment are crucial for managing HT-1 and preventing complications. Treatment typically involves a combination of dietary restrictions, medication, and, in some cases, liver transplantation.
- Dietary management: Individuals with HT-1 must follow a special diet low in tyrosine and phenylalanine, another amino acid. This may involve avoiding certain protein-rich foods and taking special medical formulas.
- Medication: A medication called nitisinone (NTBC) is often prescribed to inhibit the production of toxic byproducts of tyrosine breakdown. This medication helps reduce the risk of liver and kidney damage.
- Liver transplantation: In severe cases of HT-1 where liver damage is extensive, a liver transplant may be necessary to replace the diseased liver with a healthy one from a donor.
Conclusion
Hereditary Tyrosinemia Type 1 (HT-1) is a rare genetic disorder that requires lifelong management. Through early diagnosis, dietary restrictions, medication, and, in some cases, liver transplantation, individuals with HT-1 can effectively manage their condition and lead fulfilling lives. Close monitoring and regular medical care are essential for optimizing outcomes and preventing complications associated with this condition.
